Guidelines
These practice guidelines follow the mission of the World Association of Perinatal Medicine in collaboration with the Perinatal Medicine Foundation, which brings together groups and individuals throughout the world, with the goal of improving the ultrasound assessment of the fetal Central Nervous System (CNS) anatomy.
For further information: info@perinatalmedicine.org

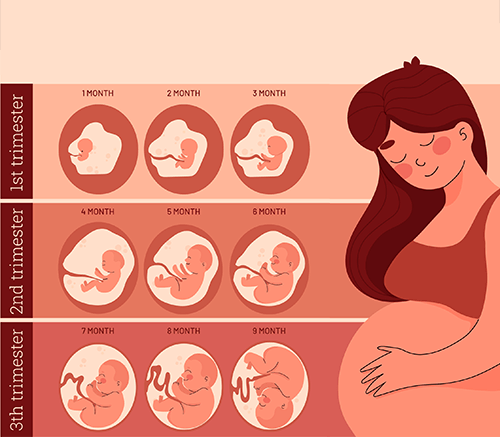
First trimester examination of fetal anatomy: clinical practice guideline by the World Association of Perinatal Medicine (WAPM) and the Perinatal Medicine Foundation (PMF)
Article info
First trimester examination of fetal anatomy: clinical practice guideline by the World Association of Perinatal Medicine (WAPM) and the Perinatal Medicine Foundation (PMF). Perinatal Journal 2022;30(2):87-102 DOI: 10.2399/prn.22.0302001
Author(s) Information
Abstract
Ultrasound in labor: clinical practice guideline recommendation by the World Association of Perinatal Medicine (WAPM) and the Perinatal Medicine Foundation (PMF)
Article info
Ultrasound in labor: clinical practice guideline recommendation by the World Association of Perinatal Medicine (WAPM) and the Perinatal Medicine Foundation (PMF). Perinatal Journal 2022;30(2):103-127 DOI: 10.2399/prn.22.0302002
Author(s) Information
Abstract

Monkeypox in pregnancy: Clinical Recommendation by the World Association of Perinatal Medicine-WAPM and the Perinatal Medicine Foundation-PMF
Article info
Monkeypox in pregnancy: Clinical Recommendation by the World Association of Perinatal Medicine-WAPM and the Perinatal Medicine Foundation-PMF. Perinatal Journal 2022;30(3):- DOI: 10.2399/prn.22.0303010
Author(s) Information
Abstract
The following recommendation aims to provide the latest evidence about the effect of MPXV in pregnancy as well as recommendations for clinical management.
The use of antenatal corticosteroids for fetal maturation: clinical practice guideline by the WAPM-World Association of Perinatal Medicine and the PMF-Perinatal Medicine Foundation
Abstract
The use of antenatal corticosteroids for fetal maturation in COVID-19: clinical practice statement by WAPM-World Association of Perinatal Medicine and the PMF-Perinatal Medicine Foundation
Abstract
WAPM-World Association of Perinatal Medicine practice guidelines: fetal central nervous system examination
Abstract
Covid-19 Study Group
With Covid-19 outbreak in these days in every country, we do try our best to overcome all problems by not just taking care of our patients at the hospital but also save and protect ourselves and our beloved ones from Covid-19. Covid-19 is challenging everything and everyone into different directions. But we have to keep ourselves active and productive even in these hectic days in our daily life. I hope you are doing well with your loved one(s).
These guidelines follow the mission of the World Association of Perinatal Medicine, which brings together groups and individuals throughout the world with the goal of improving outcomes of maternal, fetal and neonatal (perinatal) patients. Guidelines for auditing, evaluation,
and clinical care in perinatal medicine enable physicians diagnose, treat and follow-up of COVID-19-exposed pregnant women. These guidelines are based on quality
evidence in the peer review literature as well as the experience of perinatal expert throughout the world. Physicians are advised to apply these guidelines to the local realities which they face.We plan to update these guidelines as new evidence become available
Guideline for the use of antenatal corticosteroids for fetal maturation*
Women at risk of preterm birth before 34 weeks’ gestation are routinely given a course of antenatal corticosteroids (ACS) because there is good evidence that treatment reduces neonatal death, respiratory distress syndrome (RDS) and intraventricular hemorrhage (IVH)
Abstract
The aim is to present a document, which is based on current evidence and serves as a guideline for use in clinical practice. The following questions are addressed: • Is the use of antenatal corticosteroids (ACS) an effective therapy? • Who are the candidates for antenatal corticosteroid therapy? • Is there benefit after 34 weeks’ gestation? • When is the optimal time to treat? • Which are the optimal steroids; what is the ideal dose and route of administration? • Are there any contraindications to the administration of ACS? • Are antenatal corticosteroids indicated in women with premature rupture of membranes (PROM)? • Is the use of ACS recommended in pregnancies complicated by maternal diabetes mellitus? • Should the treatment with corticosteroids be repeated?
Recommendations Guidelines
The last publication of the WAPM (in cooperation with other scientific societies), Recommendations and Guidelines for Perinatal Medicine, was presented during the Congress in Florence.
INTRODUCTION
The term perinatology was introduced in 1936 by the German paediatrician Pfaundler to defi ne a period around the birth, characterize by a high fetal and neonate mortality, but with death causes different from those observed in older infants1. Perinatal medicine has as aim to improve the quality of life from its beginnings, through the fetal and newborn care. A precise terminology is required in order to describe all the events associated with perinatal outcome. International comparison of perinatal and neonatal mortality and its components is important. That information allows identifying problems, tracking temporal and geographical trends and disparities and assessing changes in public health policy and practice